Background: Older adults with hematologic malignancies have inferior survival outcomes due to multiple factors including under-treatment, drug toxicity, treatment discontinuation and concerns of frailty. However, aging is heterogeneous and chronological age is a poor indicator of underlying health. Standardizing the approach to identify frailty is an unmet need in malignant hematology. We have established a multi-disciplinary clinical model designed to identify frailty and develop personalized treatment based on objective measures of health. We have standardized a geriatric assessment (GA) model to identify vulnerability, frailty and geriatric syndromes. Here we report, the largest cohort to date, of older adults with hematologic malignancies (HM) depicting geriatric deficits and interventions with long-term clinical outcomes.
Methods: From Feb 2016 to October 2019, 311 older adults with HM were evaluated in our multi-disciplinary Cancer and Aging Resiliency (CARE) clinic. The CARE clinic is a 7-member team prescriptively evaluating the following domains: pharmacy, audiology, psychosocial needs, nutrition, physical functioning, and cognition. Geriatric syndromes were documented by CARE physician. Referral to CARE clinic is recommended for patients 60 years of age or older but all referrals are accepted independent of age. Data was abstracted by retrospective chart review. Descriptive statistics for patient characteristics, frailty measures, and prescribed interventions in each of the GA domains were provided. Univariable and multivariable Cox models were fit to associate clinical factors with OS. OS by Rockwood Clinical Frailty Scale and deficits in activities of daily living (ADLs) was evaluated by Kaplan-Meier method. Correlation between number of geriatric syndromes, clinical frailty score, and deficits in ADLs and instrumental ADLs (IADLs) was also assessed.
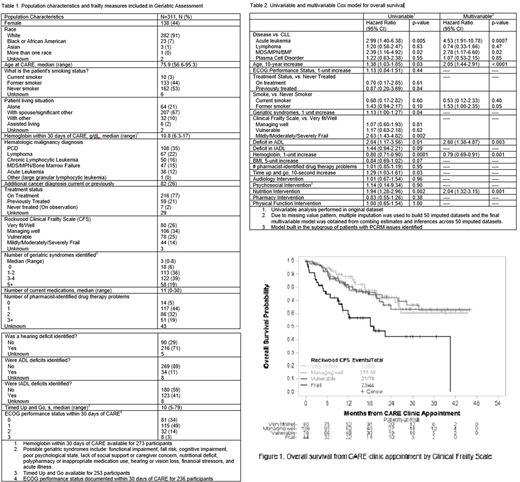
Results: Over the 42-month study period, 311 older adults with HM with a median age of 75.9 years were evaluated in CARE clinic. Key demographic features and the frequency of specific frailty measures are outlined in table 1.Geriatric interventions were common with 59% requiring 1-2 interventions and 34% requiring 3+ interventions. In univariable analysis, any degree of frailty by Clinical Frailty Scale (Hazard Ratio [HR]: 2.63, 95% Confidence Interval [CI]: 1.43-4.82, p <0.01) and increasing number of geriatric syndromes (HR:1.13, 95% CI: 1.00-1.27, p = 0.04) were associated with inferior OS. In both univariable and multivariable analyses, 10-year increase in age (multivariable HR: 2.05, 95% CI:1.44-2.91, p<0.01), deficit in ADL (multivariable HR: 2.60, 95% CI: 1.38-4.87, p<0.01), diagnosis of acute leukemia (multivariable HR: 4.53, 95% CI:1.91-10.78, p<0.01), and prescribed nutrition intervention (multivariable HR: 2.04, 95% CI: 1.32-3.15, p<0.01) were associated with inferior OS. Anemia was also associated with OS in both univariable and multivariable analysis (multivariable HR for 1 g/dL increase in hemoglobin: 0.79, 95% CI: 0.69-0.91, p<0.01). Additional variables for univariable and multivariable analyses are presented in table 2. There was significant correlation between the Clinical Frailty Scale and number of geriatric syndromes (Spearman correlation p < 0.01). The same was true of correlation between ADL or IADL deficits and Clinical Frailty Scale (p < 0.01 for both). OS by Clinical Frailty Scale and ADL deficit is pictured in figure 1.
Discussion: The Clinical Frailty Scale is predictive of OS among older adults with HM. GA-directed intervention is warranted in the vast majority of older adults with HM. In univariable analysis, Clinical Frailty Scale, increasing age, anemia, high risk HM, and increasing geriatric syndromes are associated with inferior OS. In multivariable analysis, age, anemia, and high risk HM remain significant. Nutrition and physical function are key modifiable risk factors predictive of inferior OS. Prospective studies focusing on geriatric interventions are warranted in this population with an emphasis on modifiable risk factors. This demonstrated prognostic significance of both geriatric assessments and interventions in older adults with HM should give way to future improvements in OS, quality of life, and treatment tolerability through GA-directed intervention.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal